Medication Schedule Converter
Convert confusing medication instructions into the clear Universal Medication Schedule (UMS) format. UMS uses simple time slots: morning, noon, evening, bedtime. This reduces confusion and improves safety.
Your UMS Schedule
Here's what your schedule means in the Universal Medication Schedule:
Why this works: UMS uses clear time slots instead of ambiguous phrases like "twice daily." This reduces dosing errors by 47% in elderly patients according to a 2022 study.
Tip: Always confirm your schedule with your pharmacist using the teach-back method: "Can you tell me in your own words when to take this?"
Every year, over 1.3 million medication errors happen in the U.S. alone-not because people are careless, but because the instructions on their medicine bottles don’t make sense. If you’ve ever stared at a prescription label wondering whether "take every 4-6 hours" means four pills or four hours apart, you’re not alone. Nearly half of adults misread at least one medication instruction. And when it comes to kids’ liquid medicine, the confusion gets even worse.
Why Medication Labels Are So Hard to Understand
Most prescription labels are written at a 10th-grade reading level. The average adult reads at a 6th- to 8th-grade level. That mismatch is dangerous. A label saying "Take 1 tablet by mouth twice daily" might sound simple, but it’s vague. Does "twice daily" mean morning and night? Or 12 hours apart? What if you sleep through one dose? What if you’re taking five different pills? A 2009 study found that 47% of patients misunderstood standard labels. Even when instructions were rewritten to be clearer-like "Take 1 tablet in the morning and 1 tablet in the evening"-patients with low health literacy still made mistakes 2.3 times more often than others. Why? Because it’s not just about reading. It’s about understanding numbers, measuring liquids, remembering timing, and knowing what "with food" really means. One patient in a CDC focus group said, "Every pharmacy uses different words for the same thing-I never know if 'take with food' means before, during, or after meals." That’s not a fluke. It’s the norm.What Works: The Universal Medication Schedule (UMS)
The Universal Medication Schedule (UMS) is one of the most effective tools we have. Instead of "twice daily" or "every 12 hours," UMS uses four clear times: morning, noon, evening, bedtime. No math. No guesswork. Just four times you take your pills. A 2022 study from Wisconsin Health Literacy showed that when clinics switched to UMS, dosing confusion dropped by 47% among elderly patients on multiple medications. One 72-year-old patient said, "I finally understood when to take my pills after they switched to morning/noon/evening/bedtime labels. I used to mix up my blood pressure and diabetes meds. Now I don’t." This isn’t just about convenience. It’s about safety. Taking too much of a painkiller like acetaminophen can cause liver failure. Taking too little of a blood pressure pill can lead to a stroke. UMS cuts that risk.Visuals Save Lives: Pictograms and Icons
Words aren’t enough. People with low literacy, dementia, or language barriers need pictures. A 2023 U.S. Pharmacopeia report found that labels with pictograms-simple drawings showing a person swallowing a pill, a clock, or a glass of water-increased correct understanding by 28% among patients with limited health literacy. A pictogram of a clock with "8 AM" and "8 PM" next to two pills? That’s clearer than any paragraph of text. In pediatric medicine, the difference is even starker. A 2012 review of 200 top-selling children’s cough syrups found that 63% used confusing charts like "For child 2-3 years: 2.5 mL." Parents didn’t know if that was per dose or total. Only 8% used pictograms showing a syringe with a line at 5 mL. Those parents got it right 90% of the time. The FDA is pushing for standardized pictograms on all prescription labels by 2024. That’s a big step. But right now, you can’t count on it. Always ask your pharmacist: "Can you show me how to take this?"Teach-Back: The Simple Trick That Prevents Mistakes
Doctors and pharmacists often assume patients understand because they nod and say "yes." But nodding doesn’t mean understanding. The teach-back method changes that. After explaining a medication, the provider asks: "Can you tell me in your own words when and how you’ll take this?" A 2022 study from UW Health showed this simple question reduced misunderstandings by 33%. One caregiver in a children’s hospital study said, "I thought I knew how much to give-but when I had to explain it back, I realized I had no idea what 'mL' meant." You can use this yourself. After your pharmacist gives you instructions, say: "Just to make sure I got it right-can you let me repeat it?" Then explain it out loud. If you stumble, ask again. There’s no shame in asking.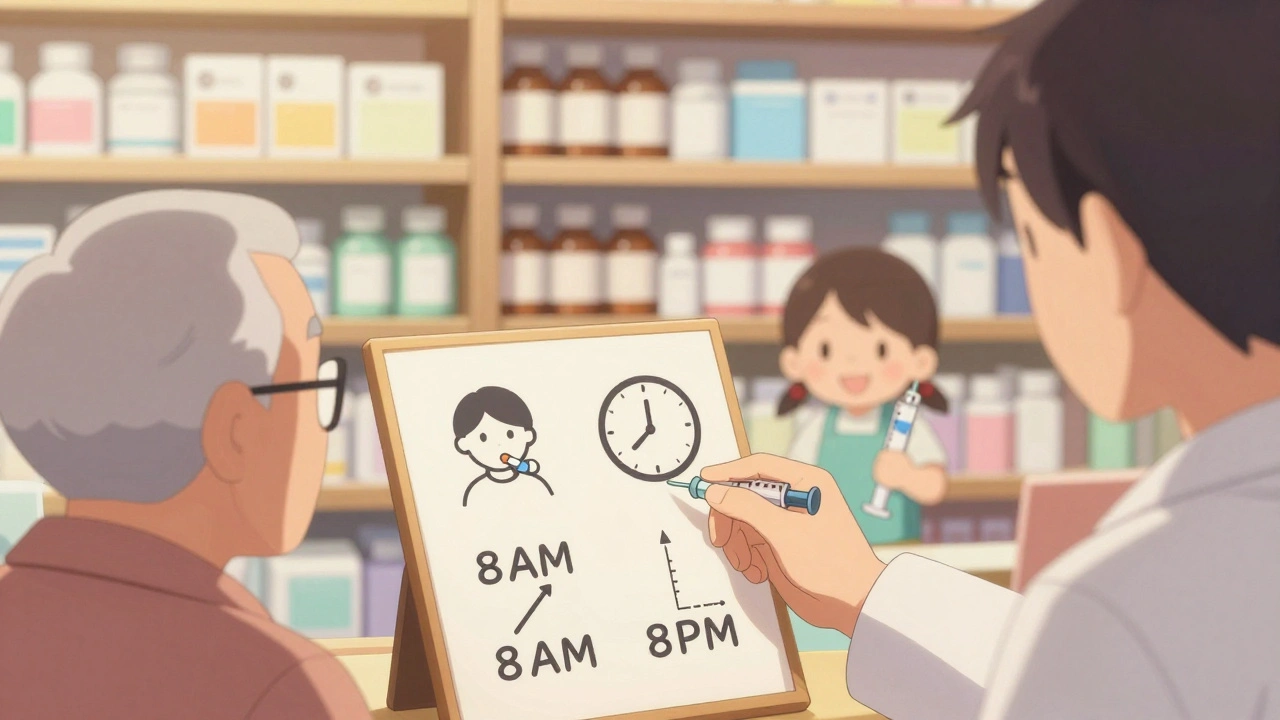
Reading Levels and Label Design
Good labels don’t use big words. They don’t use long sentences. They don’t use passive voice. The Institute for Safe Medication Practices (ISMP) recommends writing all medication instructions at a fifth-grade reading level. That means:- Average sentence length: 8 words or less
- Active voice: "Take one pill" not "One pill should be taken"
- No jargon: "Oral" → "by mouth"; "q12h" → "every 12 hours"
- One column, no clutter
- Active ingredients clearly listed on the front
What You Can Do Right Now
You don’t need to wait for the system to fix itself. Here’s what you can do today:- Ask for UMS: "Can you write my schedule as morning, noon, evening, bedtime?"
- Ask for pictures: "Do you have a visual guide for this pill?"
- Use the teach-back method: Repeat the instructions back to your pharmacist or doctor.
- Check the bottle: Is the active ingredient listed on the front? If not, ask for it.
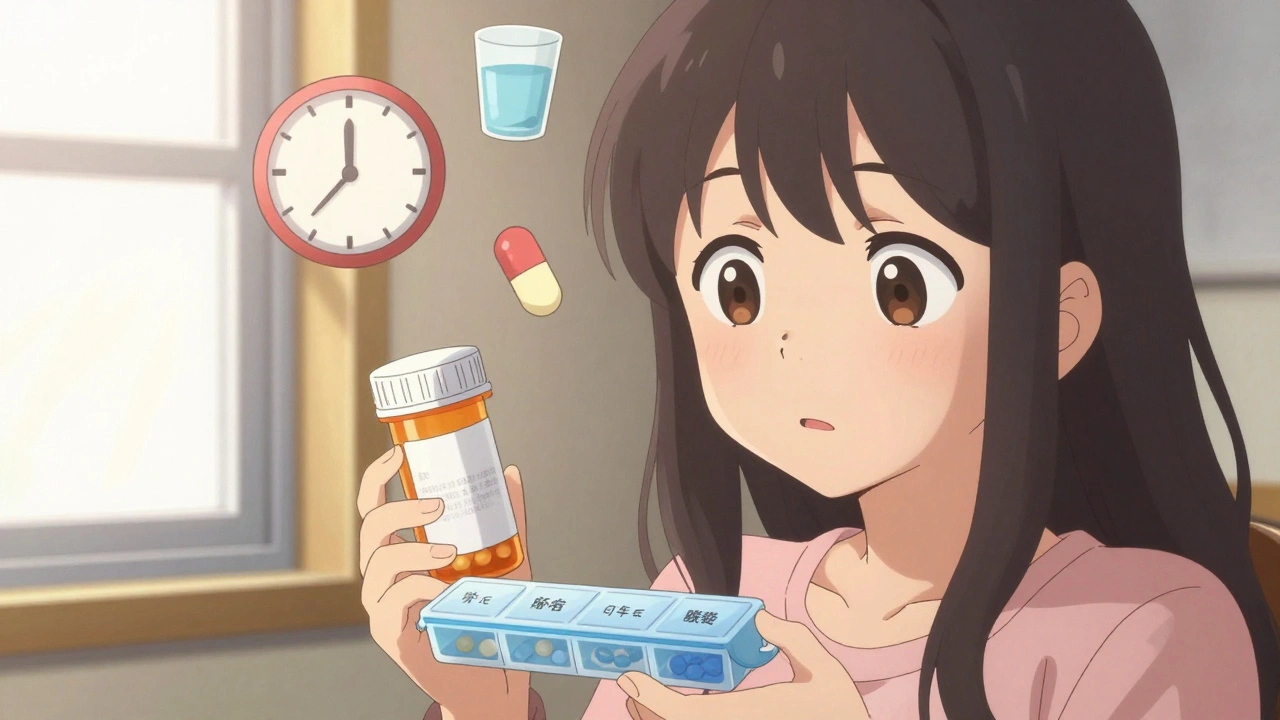
- Use a pill organizer: One compartment for each time of day. Even if you don’t need it now, it helps when you’re on more meds.
- Take a photo: Snap a picture of the label with your phone. Keep it in your notes app. You’ll thank yourself later.
Why This Matters More Than You Think
Medication errors don’t just cause side effects. They cause hospital visits, emergency rooms, and even death. A 2023 study showed that every $1 spent on health literacy tools like UMS and pictograms saves $3.75 in avoided hospital costs. And it’s not just about the elderly. Parents giving children’s medicine, people managing diabetes or heart disease, people taking antibiotics or painkillers-all of us are at risk. The truth is, the system isn’t designed for you. It’s designed for speed. For volume. For lawyers and regulators who think "clear enough" means "legally protected." But your health isn’t a legal form. It’s your life.What’s Coming Next
By May 2025, U.S. pharmacies must follow new labeling rules from the U.S. Pharmacopeia (USP). That means clearer fonts, standardized icons, and mandatory pictograms on all prescription bottles. The FDA is also requiring drug makers to test labels with real patients before they’re sold. AI tools are being developed to scan your pill bottle and explain it in plain language. But until those arrive, you’re your own best advocate.Common Mistakes and How to Avoid Them
- Mistake: "Take every 4-6 hours" → Belief: "I can take 4 to 6 pills in a day." Solution: Ask: "Does this mean I take one pill every 4 to 6 hours?"
- Mistake: "Take 5 mL twice daily" → Belief: "I give 5 mL total, split between two doses." Solution: "Is it 5 mL each time?"
- Mistake: Confusing "mg" (milligrams) with "mL" (milliliters). Solution: Always ask: "Is this measured in drops, milligrams, or milliliters?"
- Mistake: "Take with food" → Belief: "I can take it anytime I eat." Solution: Ask: "Should I take it right before, during, or after eating?"
- Mistake: "Take twice daily" → Belief: "I can take it when I wake up and when I go to bed." Solution: Ask: "Should it be exactly 12 hours apart?"
One pharmacist on Reddit said: "The most common mistake we see? Patients doubling their dose because they think 'take every 12 hours' and 'take twice daily' mean the same thing. They don’t."
Final Thought: You’re Not the Problem
If you’ve ever taken medicine wrong, don’t blame yourself. The labels are confusing. The system is broken. But you can fix it-piece by piece.Ask questions. Use pictures. Repeat instructions. Write it down. Use a pill box. Take a photo. You don’t need to be a doctor to keep yourself safe. You just need to know your rights-and how to ask for what you need.
What does health literacy mean for taking medicine?
Health literacy means being able to read, understand, and use health information to make safe decisions. For medication, that includes knowing how much to take, when to take it, what it’s for, and what to avoid. Low health literacy doesn’t mean you’re unintelligent-it means the information wasn’t made clear enough for you to understand easily.
Why do medicine labels use terms like 'twice daily' instead of 'morning and night'?
Traditional labels use medical jargon because they were designed for professionals, not patients. Terms like 'twice daily' or 'q12h' are shortcuts for doctors and pharmacists. But they’re confusing for most people. The shift to plain language-like 'morning and night'-is happening slowly, thanks to new safety standards.
Can I trust the dosing instructions on over-the-counter medicine?
Not always. A 2012 study found that 18.5% of top-selling children’s cough syrups didn’t list active ingredients on the front. Many used confusing charts instead of simple numbers. Always check the active ingredient, compare it to any prescription meds you’re taking, and ask a pharmacist if you’re unsure. Don’t assume OTC means safe.
How can I help an elderly parent understand their meds?
Use the Universal Medication Schedule: write down 'morning, noon, evening, bedtime' next to each pill. Use a pill organizer with four sections. Take a photo of each label and store it on your phone. Sit with them and use the teach-back method: "Can you show me how you’ll take your blood pressure pill?" If they can’t, go over it again. Don’t assume they know.
Are there apps or tools that help with medication safety?
Yes. Some apps let you scan a pill bottle and get plain-language instructions. Others send reminders and show pictograms. But the most powerful tool is still human interaction: asking your pharmacist to show you how to take it, using a pill box, and repeating instructions back. Technology helps-but your voice matters more.
Comments (15)
alaa ismail
December 3, 2025 AT 06:09
Been there. Stared at a bottle for 10 minutes wondering if 'every 8 hours' meant 8 AM, 4 PM, 12 AM... or if I could just take it when I remembered. UMS changed my life. Now I just think: morning, noon, evening, bed. No math. No stress.
Pharmacies should be forced to use this. It’s not that hard.
ruiqing Jane
December 5, 2025 AT 00:52
Finally. Someone said it. This isn’t about intelligence. It’s about design failure. If your product can’t be understood by the average person, it’s not a product-it’s a liability.
I’ve trained nurses to use teach-back. It’s not magic. It’s just respect. And it cuts errors by a third. Why isn’t this mandatory everywhere?
Allan maniero
December 6, 2025 AT 19:32
It’s fascinating how the medical establishment continues to prioritize legal defensibility over human comprehension. The language on these labels isn’t designed for patients-it’s designed to absolve institutions of responsibility in court. The fact that we’ve normalized this as ‘standard practice’ speaks volumes about how little we value patient autonomy in healthcare systems. I’ve seen elderly patients cry because they were too embarrassed to admit they didn’t understand ‘q12h’-and that’s not just a communication gap, it’s a moral failure.
When the FDA finally enforces pictograms and plain language, we’ll look back and wonder how we ever tolerated this. Until then, we’re all just playing Russian roulette with our prescriptions.
Zoe Bray
December 8, 2025 AT 06:54
While the UMS framework is commendable, its implementation remains inconsistent across institutional systems. The absence of standardized nomenclature in EHRs and pharmacy dispensing software impedes scalability. Moreover, without interoperability with digital adherence platforms, the efficacy of plain-language labeling is attenuated by systemic fragmentation. A holistic, regulatory-compliant, patient-centered approach requires cross-sector coordination between CMS, FDA, and pharmacy benefit managers.
Girish Padia
December 9, 2025 AT 01:46
People just don’t want to ask questions. I’ve seen my uncle take two pills because he thought 'twice daily' meant two at once. He didn’t ask. He just guessed. Now he’s on kidney dialysis. No one else is responsible but him. Stop making excuses. Read the label. If you can’t, go back. Simple.
Sheryl Lynn
December 11, 2025 AT 01:22
Oh honey, the labels are *so* 2008. It’s like they’re still printing them on parchment with a quill. I mean, have you seen the font? The passive voice? The lack of visual hierarchy? It’s a design crime. I’d rather be handed a scroll from the Library of Alexandria than one of those labels. We need Bauhaus minimalism meets emoji clarity. A pill. A clock. A banana. Done. No paragraph. No jargon. Just vibes.
Paul Santos
December 12, 2025 AT 15:34
It’s not about the label, it’s about the epistemological rupture between clinical authority and lived experience. We’ve fetishized the white coat while abandoning the patient’s phenomenological reality. Pictograms? Cute. But they’re just band-aids on a systemic wound. Until we deconstruct the hegemony of medical discourse, we’re just rearranging deck chairs on the Titanic. 🤷♂️
Eddy Kimani
December 13, 2025 AT 00:06
Interesting data, but I’m curious about the effect size across demographics. Did the UMS intervention show differential efficacy among non-native English speakers versus monolingual patients? And were the pictograms culturally adapted? A clock icon might mean something totally different in some regions. Also, what about cognitive load in polypharmacy? The 47% reduction is promising, but I’d love to see the subgroup analysis.
Chelsea Moore
December 13, 2025 AT 13:12
I can’t believe we’re still having this conversation. My grandma died because she took her blood thinner at the wrong time. She didn’t know what 'q12h' meant. And now? The pharmacy gave her a label that looked like a ransom note. I’m furious. This isn’t just negligence-it’s cruelty. Someone needs to get fired. And someone needs to go to jail.
Kristen Yates
December 13, 2025 AT 13:41
I’m from a village where people don’t read much. We used to draw dots on the calendar for each pill. Morning dot. Night dot. No words. It worked. Simple is better. Always.
Victoria Graci
December 15, 2025 AT 03:25
There’s something deeply human about the way we’ve allowed institutions to outsource responsibility for our survival onto cryptic symbols and jargon. We don’t just misunderstand labels-we misunderstand ourselves. We’ve been trained to feel stupid when we don’t get it, when the truth is, the system was never meant to be understood. The teach-back method isn’t just a tool-it’s a quiet act of rebellion. Reclaiming your body from the machine. One sentence at a time.
Saravanan Sathyanandha
December 16, 2025 AT 09:10
In my community, many elders rely on children to interpret prescriptions. But what if the child is also confused? We started a weekly 'Medication Circle' at the temple-people bring their bottles, we lay them out, and we draw pictures together. No one feels ashamed. We use sticky notes, crayons, even WhatsApp voice notes. It’s not perfect, but it’s ours. And it works. Health literacy isn’t a policy-it’s a practice we build together.
Fern Marder
December 16, 2025 AT 20:36
OMG YES. I just had to explain to my mom why 'take with food' doesn't mean 'take with your 3pm snack of chips'. She thought it meant 'if you eat, then take it'. I had to draw a timeline with emojis. 🍽️💊🌅🌙. She’s 71. She’s brilliant. But the label? A disaster. 😭
Carolyn Woodard
December 17, 2025 AT 04:37
I’ve been researching the cognitive load of medication adherence for over a decade. The problem isn’t literacy-it’s attentional fragmentation. Patients are overwhelmed by multiple regimens, multiple providers, and multiple interfaces. A simple label won’t fix that. We need integrated digital decision aids that contextualize instructions within the patient’s daily rhythm-meal times, sleep cycles, activity patterns. Otherwise, we’re just adding another cognitive burden to an already overloaded system.
Anthony Breakspear
December 17, 2025 AT 20:53
My dad used to mix up his diabetes and blood pressure meds. Then we got him a pill organizer with morning/noon/evening/bed slots. We took a photo of each bottle and labeled it with sticky notes: 'AM: blue pill for heart', 'PM: white pill for sugar'. Now he’s been stable for 2 years. No hospital. No panic. Just a box, a phone, and a little patience. You don’t need a PhD to save a life. You just need to care enough to ask.