When Two Drugs Meet: The Hidden Battle Inside Your Body
Imagine taking two pills at once - one for high blood pressure, another for pain. You think they’re just doing their jobs, side by side. But inside your body, something far more complex is happening. One drug might be fighting the other, canceling it out, or worse - teaming up to push your system over the edge. This isn’t science fiction. It’s pharmacodynamic drug interactions, and they’re responsible for nearly half of all serious drug-related hospitalizations.
Unlike pharmacokinetic interactions - where drugs mess with how your body absorbs, breaks down, or gets rid of another - pharmacodynamic interactions happen at the target site. The drug concentrations stay the same, but what they do to your cells changes. It’s like two people trying to turn the same key in a lock. One might block the other. Or they might both turn it harder than either could alone.
Three Ways Drugs Can Clash - or Team Up
Pharmacodynamic interactions fall into three clear categories: additive, synergistic, and antagonistic. Each has real-world consequences.
- Additive: The combined effect equals the sum of each drug’s individual effect. Taking acetaminophen and codeine together? You get the pain relief from both, added up. This is often intentional - doctors rely on it.
- Synergistic: The combo does more than the sum. Think of trimethoprim and sulfamethoxazole. Together, they block two steps in bacterial folic acid production. Alone, each needs a high dose. Together, they work at a quarter of the dose, cutting side effects and boosting effectiveness. This synergy is why this combo remains a first-line antibiotic for urinary tract infections.
- Antagonistic: One drug blocks or reduces the effect of another. This is where things get dangerous. Beta-blockers like propranolol can completely shut down albuterol’s ability to open airways in asthma patients. One drug is trying to help, the other is shutting the door. In some cases, this isn’t just ineffective - it’s life-threatening.
Receptors: The Battlefield Where Drugs Fight
Most pharmacodynamic interactions happen at receptors - tiny protein switches on cell surfaces. Drugs bind to them like keys in locks. If two drugs want the same lock, they compete. The one with higher affinity - meaning it sticks tighter - wins.
Take opioid painkillers and naloxone. Naloxone is designed to kick opioids off receptors during overdose. But if someone dependent on opioids gets naloxone by accident - say, from a mistaken prescription - it doesn’t just block the painkiller. It yanks it away fast, triggering sudden, violent withdrawal: sweating, vomiting, seizures. This isn’t a side effect. It’s a direct pharmacodynamic battle.
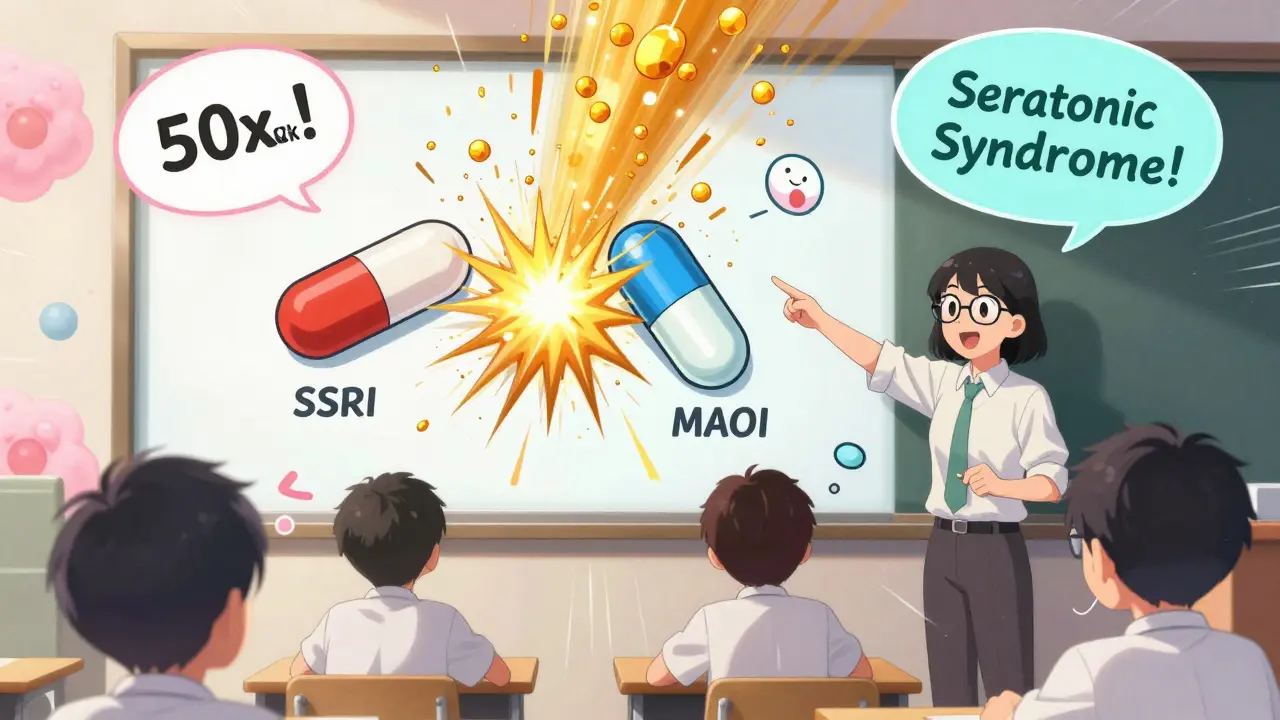
Another example: SSRIs (like sertraline) and MAOIs (like phenelzine). Both increase serotonin, but through different paths. When combined, serotonin floods the system. The result? Serotonin syndrome - high fever, muscle rigidity, confusion. A 2021 meta-analysis found this combo increases serotonin syndrome risk by 24 times. It’s not rare. Emergency rooms see it every month.
When Drugs Interfere With Your Body’s Natural Systems
Not all interactions happen at receptors. Sometimes, one drug messes with your body’s own processes.
Take NSAIDs like ibuprofen. They’re great for pain. But when taken with ACE inhibitors (like lisinopril), they blunt the blood pressure-lowering effect. Why? NSAIDs block prostaglandins - chemicals your kidneys use to maintain blood flow. Without them, kidney blood flow drops by about 25%. The ACE inhibitor can’t work properly. The result? Blood pressure stays high, even though you’re taking the pill.
Same thing happens with diuretics. NSAIDs reduce their ability to flush fluid, making them useless for swelling or heart failure. A 2019 NIH study of 347 hypertensive patients showed this interaction was present in over 40% of those taking both drugs long-term.
Even something as simple as a cold medicine can interfere. Decongestants like pseudoephedrine raise blood pressure. If you’re on beta-blockers for heart disease, that decongestant can undo months of careful control.
The Most Dangerous Combinations You Might Not Know About
Some interactions are so risky, they’re considered absolute no-gos. Here are the top three that cause the most harm:
- SSRIs + MAOIs: As mentioned, this combo can trigger serotonin syndrome. Even a few days of overlap after switching medications can be deadly. Guidelines say you must wait at least 14 days after stopping an MAOI before starting an SSRI.
- Opioids + Benzodiazepines: Both depress the central nervous system. Together, they slow breathing to dangerous levels. The CDC reports this combination was involved in nearly 30% of opioid-related overdose deaths between 2015 and 2019.
- Anticoagulants + Antiplatelets: Warfarin, apixaban, aspirin, clopidogrel - combining any of these raises bleeding risk dramatically. A 2022 survey of 1,247 doctors found 38% had seen a major bleed linked to this combo. It’s one of the most common reasons for ER visits in older adults.
And here’s a hidden one: linezolid + sertraline. Linezolid is an antibiotic, but it’s also a weak MAOI. In 2023, a hospital pharmacist posted on Reddit about a 78-year-old patient who developed serotonin syndrome after taking both. It took 72 hours in intensive care to stabilize. This isn’t a fluke. It’s a known risk - but many prescribers don’t know it.
When Interactions Actually Help
Not all pharmacodynamic interactions are bad. Medicine often uses them on purpose.
Low-dose naltrexone (LDN), originally an opioid blocker, is now being used with antidepressants for treatment-resistant depression. In a 2021 trial of 142 patients, 68% saw improvement with the combo - compared to just 42% on antidepressants alone. The theory? Naltrexone briefly blocks opioid receptors, triggering the body to produce more natural painkillers and mood-boosting chemicals.
Another example: levodopa and carbidopa. Levodopa helps Parkinson’s patients move better. But without carbidopa, most of it gets broken down before reaching the brain. Carbidopa doesn’t cross the blood-brain barrier - it just blocks the enzyme that destroys levodopa in the body. The result? More levodopa gets to where it’s needed, with fewer side effects like nausea.
These aren’t accidents. They’re carefully designed combinations. The difference? In therapeutic synergies, the interaction is intentional, monitored, and dosed precisely.

Why Doctors Miss These Interactions - And What You Can Do
Even with electronic health records and drug interaction checkers, 22% of dangerous pharmacodynamic interactions still slip through. Why? Algorithms are built for pharmacokinetic interactions - the ones you can fix with dose changes. They’re bad at spotting receptor-level battles or physiological interference.
A 2021 review in BMJ Quality & Safety found that pharmacist-led medication reviews cut adverse events from these interactions by 58% in elderly patients. Why? Pharmacists don’t just check a database. They ask: “What’s the goal of this drug?” “What’s the patient’s real condition?” “Could this be masking something worse?”
Here’s what you can do:
- Keep a written list of every pill, supplement, and OTC drug you take - including frequency and reason.
- Ask your pharmacist: “Could any of these drugs be working against each other?”
- Know your high-risk drugs: anticoagulants, antidepressants, blood pressure meds, painkillers, and antibiotics like linezolid.
- If you feel worse after starting a new drug - even if it’s supposed to help - speak up. It might not be a side effect. It might be an interaction.
The Future: Smarter, Safer Prescribing
The FDA now requires pharmacodynamic interaction studies for all new CNS drugs. The European Medicines Agency reports that 34% of new drug applications now include this data - up from 19% in 2015. Researchers are building machine learning models that predict serotonin syndrome risk with 89% accuracy.
But the real breakthrough? Real-time alerts inside electronic health records. The UK’s NHS is piloting a system that flags risky combinations as doctors type prescriptions. One hospital reported a 40% drop in dangerous interactions within six months.
Still, technology can’t replace knowledge. The most effective tool remains a clinician who understands receptors, physiology, and the patient’s full story. That’s why medical boards like CICM require doctors to memorize five key examples of each interaction type. It’s not about rote learning. It’s about building a mental map of how drugs behave in the body.
As the global population ages and polypharmacy becomes the norm - the average 65+ person takes nearly five prescription drugs - understanding these hidden battles isn’t optional. It’s essential.
What’s the difference between pharmacodynamic and pharmacokinetic drug interactions?
Pharmacokinetic interactions change how your body processes a drug - like speeding up or slowing down its breakdown in the liver. Pharmacodynamic interactions happen at the target site: drugs affect each other’s action without changing their levels in your blood. One might block a receptor, the other might boost a body system. You can fix pharmacokinetic issues with dose changes. Pharmacodynamic ones often require avoiding the combo entirely.
Can over-the-counter drugs cause pharmacodynamic interactions?
Absolutely. Common OTC drugs like ibuprofen, pseudoephedrine, and even St. John’s wort can interfere with prescription meds. Ibuprofen reduces the effect of blood pressure drugs. Pseudoephedrine can spike blood pressure if you’re on beta-blockers. St. John’s wort can trigger serotonin syndrome when mixed with antidepressants. Never assume OTC means safe.
Why are older adults at higher risk for pharmacodynamic interactions?
Older adults often take multiple medications for chronic conditions. Their bodies also process drugs differently - kidneys and liver work slower, and receptors become more sensitive. A drug that was safe at 50 might be dangerous at 75. Plus, they’re more likely to be on drugs with narrow therapeutic indexes, like warfarin or digoxin, where small changes in effect can lead to toxicity or failure.
Is it safe to take herbal supplements with prescription drugs?
Many herbal supplements interact with drugs in dangerous ways. Garlic, ginkgo, and ginseng can increase bleeding risk with blood thinners. St. John’s wort can make antidepressants, birth control, or HIV meds useless. Kava and valerian can intensify sedation from benzodiazepines or opioids. Always tell your doctor or pharmacist what supplements you take - even if you think they’re harmless.
How can I know if I’m experiencing a drug interaction?
Watch for sudden changes: new dizziness, confusion, rapid heartbeat, unexplained bleeding, or worsening symptoms. If you start a new drug and feel worse instead of better, it could be an interaction - not just a side effect. Don’t ignore it. Call your doctor or pharmacist. Bring your full medication list. Timing matters: interactions often show up within days of starting a new drug.
Final Thought: Knowledge Is Your Best Defense
Drugs are powerful. When they work together, they can save lives. When they clash, they can end them. The difference often comes down to awareness. You don’t need to be a pharmacist to protect yourself. You just need to ask questions, keep a list, and speak up when something feels off. Your body is a complex system - treat it that way.

Comments (1)
Geri Rogers
February 3, 2026 AT 01:05
OMG this is SO important!! 🙌 I work in pharmacy and see this ALL the time - people popping ibuprofen with their blood pressure meds like it’s candy. And don’t even get me started on St. John’s wort + SSRIs. One lady came in with serotonin syndrome after mixing them ‘because she heard it was natural.’ Natural doesn’t mean safe, folks. 🚨 Please, if you’re on meds, keep a list. Write it down. Show it to your pharmacist. It’s literally life or death.