Eye Cancer Radiation Therapy Selector
Select your tumor characteristics and click "Determine Best Modality"
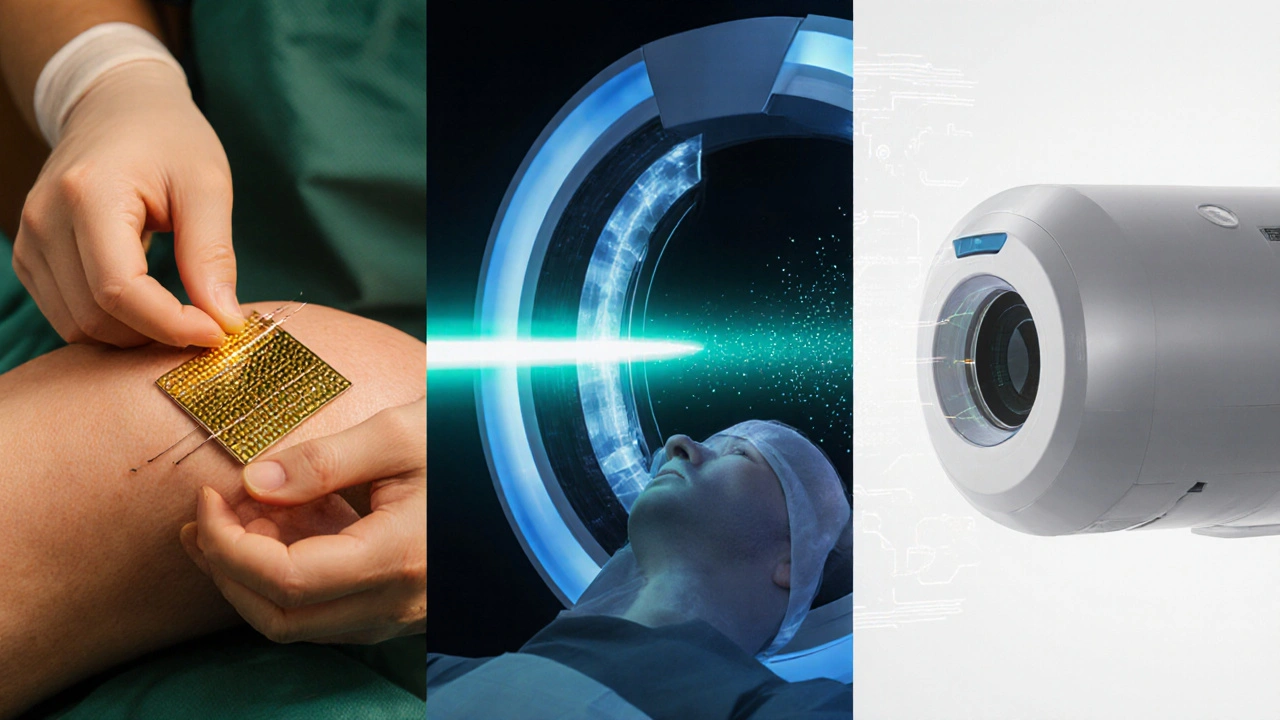
Brachytherapy (Plaque)
Best for small to medium choroidal melanomas
- 70-100 Gy total
- 3-7 day treatment
- High local control
Proton Therapy
Ideal for large or posterior tumors
- 50-70 Gy in 4-5 fractions
- Precise dose fall-off
- Excellent for posterior tumors
EBRT (IMRT/SRS)
Most accessible option
- 40-60 Gy in fractions
- Non-invasive
- Wide availability
TL;DR
- Radiation therapy uses high‑energy beams to destroy eye‑cancer cells while sparing surrounding tissue.
- Three main modalities are used: brachytherapy (plaque), proton therapy, and external‑beam radiotherapy.
- Choice depends on tumor size, location, patient age, and equipment availability.
- Treatment usually lasts 3‑7 days, followed by a gradual visual recovery period.
- Common side effects include dry eye, cataract formation, and temporary vision changes; most are manageable.
When doctors talk about radiation therapya medical treatment that delivers controlled doses of ionizing radiation to kill cancer cells, they’re referring to a tool that can target tumors inside the eye without removing the organ. Eye cancerany malignant growth that originates in ocular structures such as the retina, choroid, or ciliary body is rare, but when it occurs, preserving vision becomes a top priority. This article explains how radiation therapy works for eye cancer, walks through the main techniques, and shows what patients can expect before, during, and after treatment.
How Radiation Therapy Eliminates Cancer Cells
The core idea is simple: high‑energy particles or photons damage the DNA inside tumor cells, preventing them from dividing. Normal cells can repair this damage better than cancer cells, so the net effect is tumor shrinkage with limited collateral injury. Modern machines deliver radiation with sub‑millimeter precision, guided by imaging (CT, MRI, or ultrasound) that maps the exact shape of the tumor.
Key attributes of a radiation plan include:
- Energy type - photons, protons, or radioactive isotopes.
- Dose - measured in Gray (Gy), often split into multiple fractions.
- Target margin - a small safety buffer (usually 1-2mm) around the tumor.
These parameters are tailored by a radiation oncologista physician who designs and oversees radiation treatment plans together with a multidisciplinary team that may include ophthalmologists, medical physicists, and dosimetrists.
Radiation Modalities Used for Eye Cancer
Three techniques dominate the landscape in 2025:
Brachytherapy (Plaque Therapy)
Brachytherapy places a small, sealed plaque containing radioactive iodine‑125 or ruthenium‑106 directly on the sclera (the white of the eye). The plaque stays in place for 3‑7 days, delivering a high dose to the tumor while the rest of the eye gets far less exposure.
Typical attributes:
- Energy source: Low‑energy gamma or beta emitters.
- Typical dose: 70‑100Gy total.
- Best for: Small‑to‑medium choroidal melanomas (≤10mm basal diameter).
Proton Therapy
Proton therapy uses positively charged protons accelerated to high speeds. Because protons stop at a precise depth (the Bragg peak), they spare tissue beyond the tumor, making this method ideal for lesions close to the optic nerve or macula.
Typical attributes:
- Energy source: High‑energy protons (70-250MeV).
- Typical dose: 50‑70Gy delivered in 4‑5 fractions.
- Best for: Large or juxtapapillary melanomas, and cases where preserving central vision is critical.
External‑Beam Radiotherapy (EBRT)
EBRT directs photon beams from a linear accelerator (LINAC) at the eye. Advanced techniques such as intensity‑modulated radiotherapy (IMRT) or stereotactic radiosurgery (SRS) shape the beam to match the tumor contour.
Typical attributes:
- Energy source: High‑energy X‑rays (6‑15MV).
- Typical dose: 40‑60Gy in fractions of 2Gy.
- Best for: Patients without access to a proton center and for tumors that are not ideal for plaque placement.
Choosing the Right Modality - Decision Criteria
Doctors weigh several factors before recommending a specific type:
| Modality | Energy Source | Typical Dose (Gy) | Availability (2025) | Pros | Cons |
|---|---|---|---|---|---|
| Brachytherapy | I‑125 / Ru‑106 isotopes | 70‑100 | Widely available in ophthalmic centers | High local control; short treatment period | Surgical plaque placement; risk of radiation‑induced cataract |
| Proton Therapy | Protons (70‑250MeV) | 50‑70 | Limited to ~30 centers worldwide | Precise dose fall‑off; excellent for posterior tumors | Travel required; higher cost |
| EBRT (IMRT/SRS) | High‑energy X‑rays | 40‑60 | Most common in radiation centers | Non‑invasive; no surgery | Potentially greater exposure to surrounding tissue |
In short, small peripheral tumors often go with brachytherapy, large posterior lesions lean toward proton therapy, and EBRT serves as an accessible fallback.
Step‑by‑Step: What Happens During Treatment
- Simulation & Planning: A CT or MRI scan captures the eye’s anatomy. The radiation oncologist, together with a medical physicist, draws a 3‑D contour of the tumor and critical structures (optic nerve, lens).
- Custom Device Creation (if needed): For plaque therapy, a custom‑shaped silicone insert holds the radioactive seeds. For proton therapy, a patient‑specific aperture is milled.
- Positioning & Immobilization: The patient rests on a chin‑rest with a bite‑block or a customized mask to keep the eye perfectly still.
- Delivery: Depending on modality, the radiation is emitted for a few minutes (EBRT/SRS) or the plaque remains surgically attached for several days (brachytherapy). Proton sessions last ~5‑10 minutes each.
- Post‑Treatment Monitoring: Follow‑up visits at 1month, 3months, then every 6months for at least 5years. Imaging checks tumor regression and eye health.
Managing Side Effects - What to Expect
Because the eye is delicate, even precise radiation can cause short‑ and long‑term changes. Common issues include:
- Dry eye - due to reduced tear production; artificial tears and punctal plugs help.
- Cataract formation - especially with plaque therapy; surgery is often required later.
- Radiation retinopathy - delayed vascular damage; treated with anti‑VEGF injections.
- Vision fluctuations - many patients notice blurry vision for weeks; improves as swelling subsides.
Early referral to an ocular oncologist and a low‑vision specialist can preserve quality of life. Lifestyle tweaks-protecting the eyes from bright light, using sunglasses with UV protection, and maintaining good blood pressure-also reduce risk.
Outcomes & Prognosis
When radiation therapy is applied appropriately, local control rates exceed 90% for most ocular melanomas. Studies from the International Ophthalmic Oncology Society (2023) show a 5‑year eye‑preservation rate of 78% for plaque therapy and 84% for proton therapy. Visual acuity after treatment depends heavily on tumor location; tumors away from the macula often retain 20/40 vision or better.
Importantly, radiation does not replace systemic chemotherapy for metastatic disease. If the cancer spreads beyond the eye, a multidisciplinary approach-including immunotherapy agents like pembrolizumab-becomes necessary.
Frequently Asked Questions
Is radiation therapy painful?
The procedure itself is painless. During plaque placement you receive a brief local anesthetic, and during external‑beam sessions you lie still on a table. Any discomfort usually comes from eye irritation after treatment, which is manageable with eye drops.
Can I keep working while receiving radiation?
Yes. Most patients resume normal activities within a day or two after each session. Brachytherapy does require a short hospital stay for the plaque duration, but many centers allow outpatient care.
What is the success rate for preserving vision?
If the tumor is small and located away from the central macula, more than 80% of patients retain useful vision (20/40 or better). Larger or centrally located tumors have lower rates, but many still avoid total blindness.
Do I need a specialist for follow‑up?
Yes. Ocular oncology clinics provide regular imaging and eye exams to catch complications early. Coordination between the radiation oncologist and ophthalmologist is essential.
How much does radiation therapy for eye cancer cost?
Costs vary by country and modality. In the U.S., plaque therapy averages $15,000-$25,000, proton therapy can exceed $40,000, and EBRT typically falls between $10,000-$18,000. Insurance often covers a large portion when the indication is cancer.
Understanding the role of radiation therapy eye cancer helps patients weigh benefits against risks and choose a path that aligns with their visual goals. With modern imaging, precise delivery, and supportive eye‑care, radiation remains the cornerstone of curative treatment for most eye‑based malignancies.

Comments (18)
Keyla Garcia
October 3, 2025 AT 10:16
💥 This guide breaks down eye‑cancer radiation like a blockbuster plot twist! Small tumors = quick plaque, big ones = proton power. 😱 Your eyeball stays the star, not the villain.
Ismaeel Ishaaq
October 7, 2025 AT 08:51
Yo, the options are as vibrant as a sunrise over Lagos! You can slap a tiny plaque and be done in a week, or book a trip to a proton hub and chase that remission like a champion. Keep that optimism blazing, fam!
Jesse Goodman
October 11, 2025 AT 07:27
Radiation reshapes reality; the eye finds balance amid photons. 🌟
Antara Kumar
October 15, 2025 AT 06:02
While the article praises proton centers abroad, India has capable facilities that deserve recognition. Don't let western hype dictate your treatment choice.
John Barton
October 19, 2025 AT 04:37
Oh great, another fancy tech guide-because we all have time to book flights to a proton palace while our vision fades, right?
Achint Patel
October 23, 2025 AT 03:13
In the grand tapestry of medicine, radiation threads through both hope and risk. The plaque sits like a humble monk, the proton beam a swift samurai-each with its own destiny.
Lilly Merrill
October 27, 2025 AT 00:48
I appreciate how the guide lays out the pros and cons without overwhelming jargon. It really helps patients and families make an informed choice.
Kimberly :)
October 30, 2025 AT 23:23
Sure, the guide says EBRT is the fallback, but sometimes the ‘fallback’ is actually the smartest move 😏. Trust the local team if they know your case.
Sebastian Miles
November 3, 2025 AT 21:59
From dosimetry to fractionation, the protocol aligns with AAPM TG‑138 standards, ensuring reproducible outcomes.
Harshal Sanghavi
November 7, 2025 AT 20:34
Yeah, because nothing says ‘relax’ like lying still for minutes while a machine zaps your eye-so soothing, right?
Duke Gavrilovic
November 11, 2025 AT 19:09
The comparative table succinctly captures the essential parameters, facilitating a clear decision matrix for clinicians and patients alike.
Abby VanSickle
November 15, 2025 AT 17:44
While the data underscores high preservation rates, we must not overlook the psychological toll on patients confronting potential vision loss.
chris macdaddy
November 19, 2025 AT 16:20
Yo man, ths therapy sound kinda scarry but if u got good docs it’ll b ok. just keep ur eyes clean and follow up.
Moumita Bhaumik
November 23, 2025 AT 14:55
Don't be fooled by the glossy brochures-big pharma and elite hospitals push proton therapy to keep profit flowing, not to save eyes.
Sheila Hood
November 27, 2025 AT 13:30
If you think side effects are minor, try reading the fine print; they'll surprise you with a cascade of dry‑eye woes.
Louie Hadley
December 1, 2025 AT 12:06
Ultimately, the best path blends medical expertise with the patient’s personal values, ensuring both safety and peace of mind.
Ginny Gladish
December 5, 2025 AT 10:41
The article pretends neutrality but subtly nudges readers toward high‑cost proton therapy, ignoring socioeconomic barriers. A toxic bias emerges when the prose emphasizes cutting‑edge tech without addressing access disparity. Moreover, the risk section downplays radiation retinopathy, which can cripple vision years later. Such omissions betray a commercial agenda. Readers deserve a frank discussion of both financial and long‑term health implications.
Faye Bormann
December 9, 2025 AT 09:16
I’ve read countless medical guides, and this one is oddly thorough, almost to a fault. While it praises every modality, it conveniently skips the cultural context of where patients actually live. For example, in many rural areas, traveling to a proton center is a logistical nightmare that the article barely acknowledges. Meanwhile, the superbly detailed table makes the reader feel educated, yet it subtly pushes the high‑tech options as the default. The risk profile is presented with a polite smile, ignoring that dry eye and cataracts can dramatically affect quality of life. I find it contradictory that the guide celebrates cutting‑edge technology while glossing over the sheer cost and insurance hurdles. Patients deserve transparent info about potential out‑of‑pocket expenses that can run into tens of thousands of dollars. Also, the emotional toll of waiting for treatment outcomes is mentioned only in passing, which feels dismissive. The recommendation algorithm seems to favor centers that have the equipment, not necessarily the best outcome for the individual. It’s refreshing, however, that the piece does include a set of practical after‑care tips for managing dry eye. That said, those tips are generic and could apply to any ocular condition, not just radiation‑induced changes. From a patient’s perspective, the guide could have highlighted support groups and counseling services more prominently. In short, while the technical data is solid, the narrative leans toward a sales pitch for advanced radiation. If you’re looking for a balanced view, you’ll need to consult additional sources beyond this article. Remember, the best treatment is the one that fits your medical needs, financial situation, and personal comfort level.